I am at the AIBD conference in Orlando. This is probably the premiere clinical practice conference in the US. No chance getting to Disney World, there is just too much conference to go to!
This will be a combo blog as well as some various thoughts driven by the conference.
At the moment (1:30 on Thursday 12/12/19) I’m at an interesting conference about patient stratification for IBD. The message here (by Corey Siegel, MD) is that some patients are at high risk for severe disease. In Crohn’s, Small bowel disease, perinatal disease, ASCA level, CBir1 level, and presence of NOD 2 mutation predict more severe disease. Using systems dynamics Analysis suggests whether a patient should consider getting biological therapy early in their disease course to prevent anticipated complications. This analysis gives a predicted course of progress of the illness and informs choices for early use of or not needing biologics.
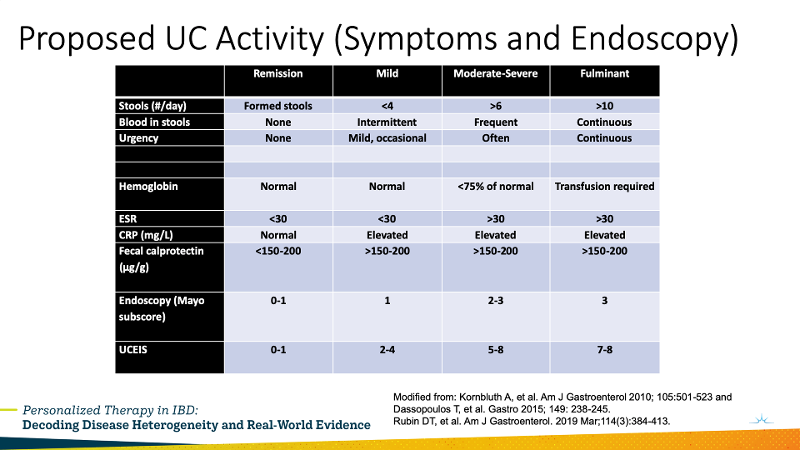
Additionally, he showed a slide adapted from the literature about current recommendations for assessing disease severity in UC.
1:40: Millie Long, MD case presentation: UC risks are onset at young age, pan-colitis, need for steroids. A patient with moderate to severe colitis, with moderate on colonoscopy between the flares she gets each fall. A young patient with years of activity of pan-colitis. This would be a good patient for a biologic. Vedolizumab was chosen with significant improvement.
Severe Perianal Disease. 2:18 Case discussion of severe perianal disease in a male. Some rectal disease. Maximize medical therapy, Push Infliximab to a level of 20. Perianal disease gets infliximab primarily. Dr. Karnbluth advocated that the surgeon needs to be an IBD experienced surgeon. Surgeons want luminal disease control first, then treat by drainage when complex, but tend to be conservative due to concern over complication risk.
2:54 Stem cells in Fistulas. There was a paper last year at DDW that used stem cell injections into perineal fistulas. This looks like it will work. It is still experimental, but with effectiveness of 50-80% it is looking good.
3:15 Malignancy with Crohn’s. When malignancy arises stop Infliximab and 6-MP. While interrupting therapy is a problem, stopping and restarting after treatment of the malignancy is generally recommended. This is mostly due to studies having excluded patients with malignancy. There is a risk of immunogenicity on restarting the infliximab.
The experts recommend that in patients on immunosuppressants go ahead and have seen by a dermatologist. This is for melanoma risk. A patient with Crohn’s was discussed, who developed a squamous cell ca. Stopping the azathioprine was suggested based on a small study showing small increase in risk of complications of the squamous cell ca. Basal cell ca doesn’t seem to be worsened by azathioprine. But the experts recommend starting a biological for 6 months before stopping the azathioprine to prevent flares.
Tofacitinib is associated with non-melanoma skin cancer.
Continue the Dermatologist screening long term even if drugs stopped.
Lymphoma: Patient developed T cell lymphoma on immunosupression therapy. Anti-TNF needs to be stopped with lymphoma. She was switched to Vedolizumab and did well. Even had a second child!
ECCO Keynote Speaker: Lessons from ECCO
Thursday, December 12, 2019 from 4:15 pm to 4:45 pm
Séverine Vermeire, MD
University hospitals Leuven and KU Leuven university
She advocated that we check TPMT.
Optimize anti-TNF. Europeans are not recommending routine therapeutic drug monitoring. (I think this is outdated. There are studies that support it. I suspect the Europeans will change.) But in patients that lose their response doing therapeutic drug monitoring is recommended. They had a study that showed no benefit of proactive drug monitoring. That said, the speaker then described a very sophisticated use of therapeutic drug monitoring.
Keynote Speaker: Lessons Learned from Functional GI: Understanding and Treating IBS in IBD
Thursday, December 12, 2019 from 5:05 pm to 5:35 pm
William Chey
Michigan Medicine
IBS is a heterogeneous disease that is affected by activation of the GI immune and enteric nervous system.
There is an overlap between IBS and IBD symptoms. Of IBS patients that meet Rome II criteria only 2 of 500 will have IBD. So it is very low, but not zero. However, 30-40% of IBD patients have IBS symptoms.
While we may not have a cure we have treatments that will allow patients to take back control of their lives.
He recommends an integrative approach: Diet, Followup with pharmacotherapy and stress management. Psychological treatments.
Glutamine has been effective in post infectious IBS.
Probiotics have been effective in IBS as well. The variety of probiotics is huge, but we don’t know which probiotic to use, since there are so many probiotics used, and we don’t know which one.
Leverage of microbiome or metabolome may be key.
Peppermint oil works as a smooth muscle relaxant. Uncharted peppermint oil drives GERD, so a coated preparation should be used.
5-HT3 antagonists are beneficial. Aldosterone was good but pulled. Ondansetron for IBD-D, 4-8 mg tid.
Eluxadoline available at 75 or 100 mg, don’t use in drinkers over 3 per day or after cholecystectomy. Pancreatitis and SOD dysfunction have been seen.
Rifaximin effective in multiple controlled trials. Only a 105 clinical improvement. 1/3 patients had a durable improvement. 2/3 needed longer therapy. No adverse effects seen compared to placebo.
Neuromodulators also effective. Tricyclics are not good anxiolytics, so an SSRI should be considered in that group.
Cool + for the post